Our success rates
(based on data from 2022)
All our patients, and prospective patients, enter treatment hoping for a successful outcome. Choosing a clinic to support you on your journey can be a difficult decision.
We know that patients will use the success rates of various clinics to help inform their decision and we therefore try to be as open as possible about the data we present. What you should bear in mind is that our individual clinic success rates cannot tell you how likely you are to have a baby. There are so many variable factors involved and a consultation with a doctor as your initial appointment can help to provide you with some extra clarity taking all of your personal circumstances into account.
What is included in, or excluded from, our data?
The data in this information leaflet is all based on the same sample of treatments. The sample does not include any patients using donor eggs, or those who have used any form of pre-implantation genetic testing (such as PGT-A, PGT-M, PGT-SR). It includes treatments where donor sperm has been used. Below we explain why these groups are excluded.
The age of the egg at the time of collection can impact on the success of the treatment. Female fertility will continue to decrease every year, whether or not someone is healthy and fit, because the number and quality of the eggs decreases with age. Current professional guidelines state that eggs should not be taken from donors aged 36 or over. In 2022 the average age of egg donors used in treatment in our Clinic was 29. As a result, we have removed treatment cycles using donor eggs from this data. This gives you a truer representation of the treatment success rates for people in your age category using eggs of the same age as yours, as it would otherwise give a misleading impression of higher success rates.
The Human Fertilisation and Embryology Authority (HFEA) classes PGT-A (pre-implantation genetic testing for aneuploidy) as a treatment add-on. This means that there is not enough evidence to show that it is effective at improving the chances of having a baby for most fertility patients. Whilst PGT-A does not carry any additional known risks for the person undergoing fertility treatment, it is known to carry some risks for the embryo. As a result of the existing scientific uncertainties, and unless otherwise clinically indicated, PGT-A is not routinely used in treatment for everyone at our Clinic. This is why cases where we have performed PGT-A are excluded from the general data presented in this leaflet, as it would otherwise give a misleading impression of higher success rates.
If you have specific questions regarding treatments using donor eggs or PGT you should ask for a consultation with a member of our clinical team.
How are the results calculated?
A positive pregnancy is confirmed with either a urine or blood test. A pregnancy test kit that you can buy at a local pharmacy is sufficient.
A clinical pregnancy is confirmed only after a fetal heartbeat has been seen on an ultrasound scan at around 6 to 9 weeks of pregnancy (i.e. not just the presence of a positive pregnancy test).
We use two measures when discussing Clinical Pregnancy Rates. One measure is “per embryo transfer” i.e. it counts how many ‘embryo transfer procedures’ have been done and the resultant pregnancy rate, regardless of the number of embryos transferred at each procedure. The other is “per embryo transferred” i.e. it counts how many ‘embryos have been transferred’ overall and the resultant pregnancy rate, regardless of how many embryos were transferred at the same time.
Transferring more than one embryo at a time does not result in a greater chance of pregnancy overall. But limiting the number of embryos that are transferred simultaneously in each treatment means that there is a much smaller chance of you having a multiple pregnancy. This reduces the risks involved to both you and your babies. We have guidelines in place to reduce the risk of multiple pregnancies and our team will give you the best advice about the number of embryos to be transferred.
Early Pregnancy Loss calculates the percentage of positive pregnancy tests that do not result in a fetal heart being seen at the early pregnancy ultrasound scan.
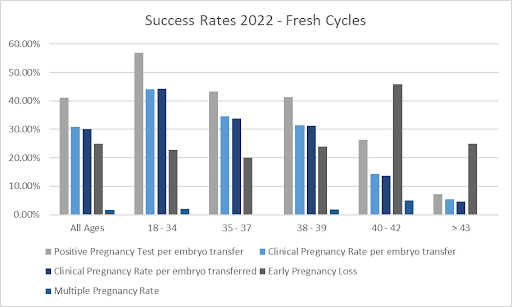
Treatments involving a fresh embryo transfer
The graph and tables below show the chances of each of the above outcomes following a fresh embryo transfer cycle.
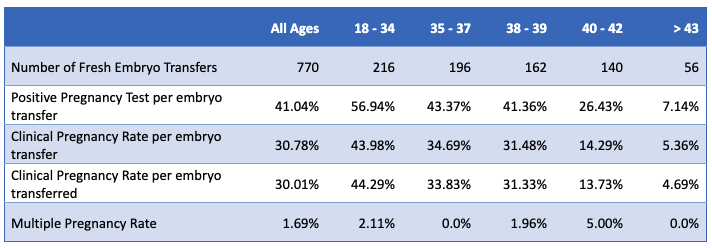
We closely monitor outcomes and advise you on the number of embryos to have transferred in order to maximise your chances of a healthy singleton pregnancy. This often results in surplus embryos following your treatment. If these embryos have been graded as being of a good quality, it is recommended that you freeze them for potential use in the future.
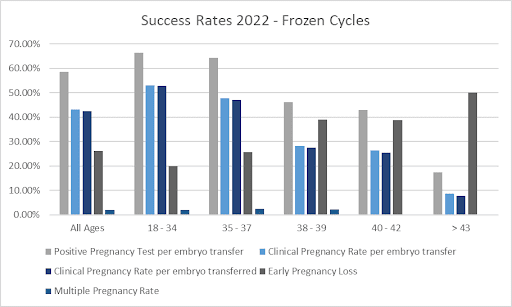
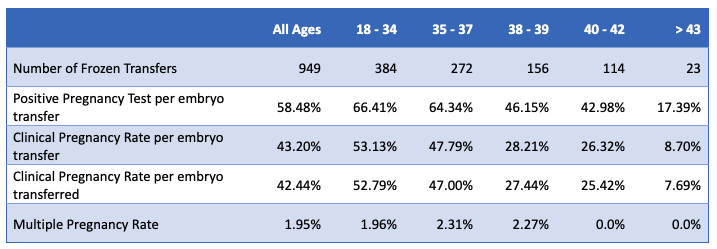
Treatments involving a frozen embryo transfer
The graph and tables below show the chances of a clinical pregnancy following a frozen embryo transfer cycle (FET). This is based on the age of the egg at the time it was collected and then frozen – not at the age the patient was when they had the transfer.
Ultimately, the aim of our treatments is for these to result in the live birth of a baby. We calculate our live birth rate compared to the number of embryos transferred. Once a fetal heartbeat is seen on an early pregnancy scan, patients are discharged from our clinic and into the care of antenatal services.
As we do not get involved in the antenatal care and deliveries of our patients, we contact all patients and hope that they will keep us up to date and provide us with information on the outcome of their pregnancy. We are not automatically provided with this by the NHS. Therefore, unless we have been informed of a child’s birth as a result of our treatment, this birth outcome cannot be included in our live birth rate figures and therefore makes them less accurate.
Furthermore, the length of a pregnancy means that this data lags by a year behind our most recent pregnancy rates. Therefore, our most recent complete set of live birth data is for 2021, as we are not able to collect yet all the live birth data resulting from our treatment cycles that started in 2022.
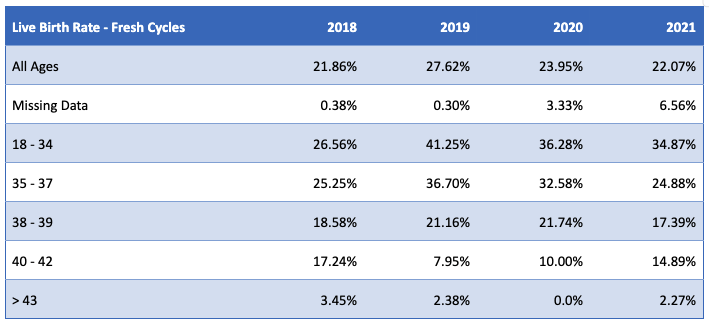
The table below shows the live birth rate that resulted following a fresh embryo transfer cycle. Please note that we have also included the percentage of data that we are missing, due to patients being ‘lost to follow-up’ and therefore being unable to verify the live birth data. These cases are automatically classed as ‘negative for live birth’, even if a baby has been born as a result of our treatment.
* Please note that for 2021 a significant proportion Live Birth of data is still outstanding
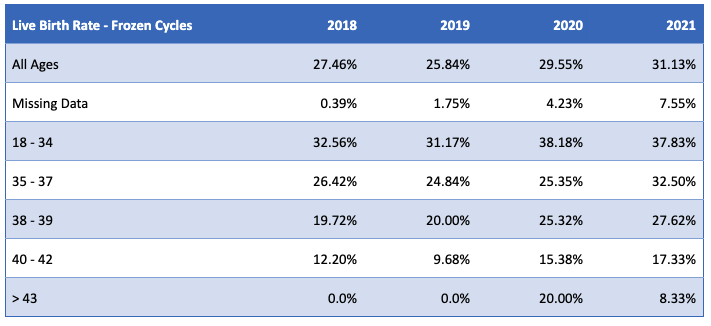
The table below shows the live birth rate that resulted following a frozen embryo transfer cycle (FET). Please note that we have also included the percentage of data that we are missing, due to patients being ‘lost to follow-up’ and therefore being unable to verify the live birth data. These cases are automatically classed as ‘negative for live birth’, even if a baby has been born as a result of our treatment.
* Please note that for 2021 a significant proportion Live Birth of data is still outstanding
Treatments using Pre-implantation Genetic Testing (PGT)
Whilst we have excluded cases where we have performed pre-implantation genetic testing (PGT) from the general data presented in this leaflet, as it would otherwise give a misleading impression of higher success rates, we nevertheless want to be informative about its use in our Clinic and its outcomes.
Between October 2020 and September 2022, we biopsied 1101 embryos for 231 patients. Approximately 80% of the biopsies were performed on eggs collected when the patient was 35 or over.
Of the 1101 embryos biopsied, 472 (42.9%) had a result consistent with a euploid embryo and therefore can be transferred. A further 28 embryos (2.5%) were classed as low mosaic (these can also be considered for transfer). A total of 553 embryos (50.2%) were classed as not being suitable for transfer due to various chromosomal abnormalities (such as being aneuploid embryos, complex aneuploid etc). Of the remaining embryos, 21 (1.9%) produced a non-informative result, and 27 (2.4%) had no DNA detected. These can either be transferred or re-biopsied as indicated.
Due to the nature of the biopsy procedure and the requirement to wait for the results, all biopsied embryos need to be frozen before a decision for a transfer can be made. Therefore, all biopsied embryos are transferred in a frozen embryo transfer cycle.
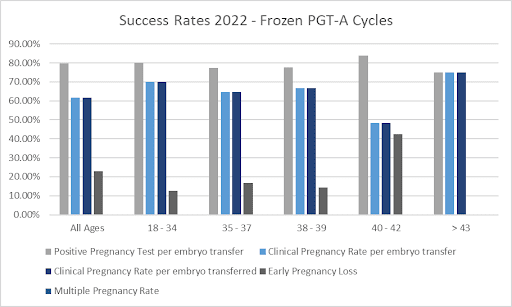
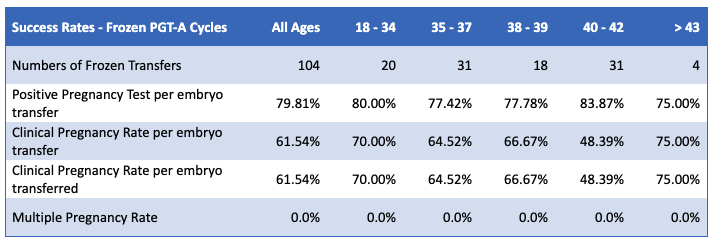
The graph and table below show the chances of each of the outcomes that resulted following a frozen embryo transfer cycle (FET) in 2022 of an embryo following PGT. This is based on the age of the egg at the time it was collected and then frozen – not at the age the patient was when they had the transfer.
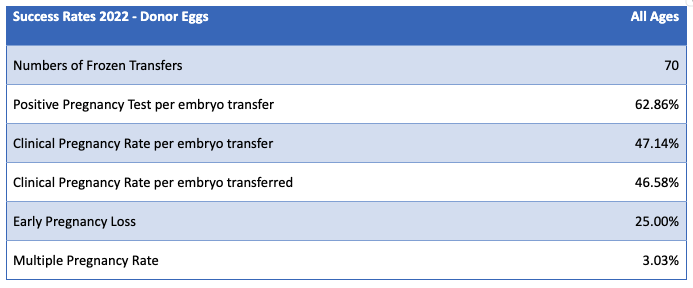
Treatments using donor eggs – success rates
As the age of the egg at collection can impact on the success of the treatment, we have excluded cases where donor eggs were used in treatment from the general data presented in this leaflet, as it would otherwise give a misleading impression of higher success rates. Below we present separately our data regarding egg donation and its outcomes at our Clinic.
In 2022 the average age of the egg donors used in treatment in our Clinic was 29.
The following table provides you with information on treatments where donor eggs were used. The majority of our egg recipient cycles in 2022 (98.5%) were of transfers involving the use of fresh donor eggs followed by an asynchronous recipient frozen embryo transfer. The rest were fresh embryo transfers in synchronized recipient cycles.
The table below shows the chances of each of the outcomes that resulted following an embryo transfer cycle (FET) that used donor eggs and were not biopsied for PGT.
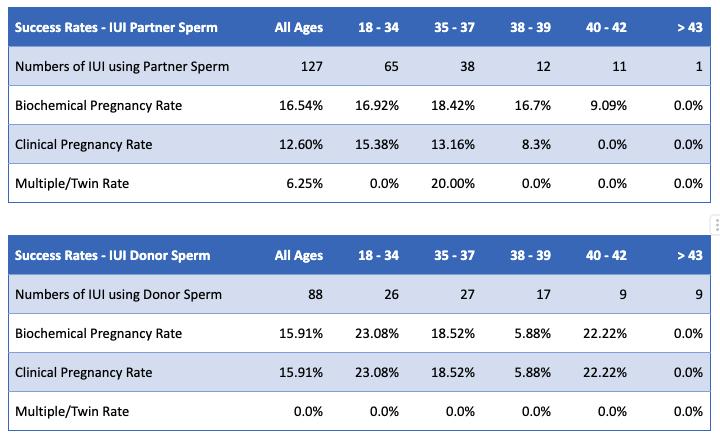
Treatments involving Intrauterine Insemination (IUI)
The table below shows the chances of each of the outcomes that resulted following an IUI cycle in 2022 and whether the patients used partner or donor sperm.
As an HFEA licensed clinic, we are required by law to provide the HFEA with our fertility treatment details and outcomes data. They store this in their register, thought to be the largest database of fertility treatment in the world. In 2021, the HFEA launched a new data submission system for clinics and migrated their data to a new database. This means they now need to upgrade their systems to enable them to make better use of their data for patients, clinicians and researchers – this work is due to be completed in winter 2022/23. This means that at present they are unable to produce data which allows you to compare clinics on an exact like for like basis.
It is important to point out that using the type of information presented in our leaflet to make comparisons between centres is of limited value. Simple general statistics do not account for how many medically complex cases a clinic treats, nor does it individualise one’s chances of success. Each person has unique, and sometimes very different requirements and reasons for seeking fertility treatment. For a more personalised estimation of your chance of success, a medical assessment is required.
Please do not hesitate to contact us should you require more detailed information about your individual chances of success at King’s Fertility.
